CRS' solutions are provided to all types of providers, including for-profit and not-for-profit hospitals, and physician groups.
CRS offers flexible fee arrangements, from full contingency to reasonable hourly rates.

Disproportionate Share (DSH) and Low Income Patients (LIP)
Hospitals receive additional reimbursement from the Medicare program for treating a disproportionate share of Medicaid eligible patients. Inpatient Rehab Facilities and hospital sub-provider rehab units receive an additional payment for treating low-income patients.
CRS Solution: CRS' executive team has performed DSH/LIP reviews for more than 20 years. CRS has experience in more than 35 states, and has access to Medicaid eligibility in 42 states. CRS documents all allowable Title XIX eligible days, provides audit support documentation and assists the provider through audit and settlement.

CRS offers concurrent and retrospective DSH reviews. Concurrent DSH reviews performed within the Medicaid program's timely filing limit, allows the provider to realize Medicaid revenue for claims identified as Medicaid through the concurrent DSH review process that were not identified as Medicaid during the registration process. CRS will prepare reopening requests for retrospective reviews and will assist the provider in filing DSH appeals.
If your organization has already performed internal DSH reviews, or if the function was contracted to an outside consultant, CRS will perform a retrospective DSH review on a fully contingent basis.
Post-acute Care Transfer (PACT)
Hospitals receive a reduced DRG payment if a patient transfers to another post-acute care facility and, if the patient's length of stay (LOS) is one day less than the geometric mean LOS.
CMS implemented the PACT policy, formerly known as The Special 10 DRG Rule, for discharges occurring on or after 10/1/1998 consisted of 10 transfer DRGs. For discharges occurring on or after 10/1/2003, the number of transfer DRGs increased to 29. Currently, the PACT policy includes 273 transfer DRGs.
CRS Solution: CRS has hassle-free, no password connectivity to the Medicare CWF. CRS reviews all transfer cases including Medicare Advantage claims, not just those DRGs subject to the PACT policy, identifies claims for rebilling, follows up with all post-acute care providers to determine if follow-up care was provided within the appropriate statutory time-frame and provides billing/follow-up support to providers. CRS reviews claims on a concurrent basis and on a retrospective basis (4-years from a claim's original determination date).

Revenue Lift Services
Many providers do not have a consistent eligibility verification screening process. A typical claim lifecycle utilizes multiple vendors, each with distinctive levels of intricacy and fees, causing clients to fail to bill claims.
Hospitals, health systems, physician practices and pharmacies may not be aware of all possible sources of health coverage payments at the time of billing - the unknown sources of health coverage payments often provide increased payments of 50% to 100%. CRS is able to identify eligibility not identified through traditional eligibility services and is able to pursue collections past typical timely filing limits.
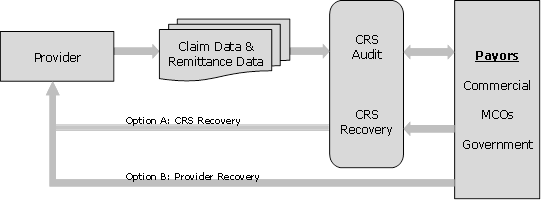
CRS Solution: CRS employs proprietary algorithms and connectivity to payors, maximizing the identification of recovery opportunities. CRS has connectivity to nearly 100% of external payors. CRS offers options for recoveries to be collected by CRS or provider. Results are typically realized within 30 to 90 days for claims submitted within the timely filing limit. Claims beyond timely filing limits may take longer depending on the payors and state regulatory environment.
Minimum support is required by the provider's business office. This is truly found money that has not been previously identified. CRS is able to accept data in nearly any format through our secured data center's HIPAA compliant data exchange.
CRS' Yield management process designed to monitor the outcome of billings and maximize recoveries.
Additional Third Party Reimbursement Services
CRS provides Medicare providers with access to individuals with extensive experience in the following areas of Medicare/Medicaid reimbursement services:


